39 year old with ascites
December 07, 2023
This is a case of a 39 year old bus driver who is a resident of West Bengal.
CHIEF COMPLAINT:
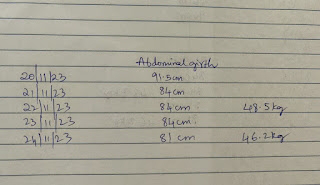
Abdominal distension since 2 months.
Swelling in the leg since 2 months.
Decreased appetite since 2 months.
Decreased urine output since 1 month.
HISTORY OF PRESENT ILLNESS-
Patient was apparently asymptomatic 2 months ago then he developed abdominal distension which was insidious in onset and gradually progressive, associated with decreased appetite. Later he developed bilateral pedal edema extending upto the knees which is of pitting type.
After a month his urine output got decreased still he continued his work as a bus driver.
His relatives started noticing that his abdomen is getting distended and his appetite is decreased.
They suggested him to see a doctor following which he took a homeopathic treatment in West Bengal But there was no improvement. He also took some ayurvedic medication but nothing seemed to work out. Then he came to our hospital with complaints of abdominal distension,pedal edema and decreased appetite.
No history of fever, breathlessness, cough
No h/o drowsiness, loss of consciousness, palpitations, orthopnoea,pnd ,abdominal pain, fever,nausea vomiting.
PAST HISTORY:
Not a known case of diabetes mellitus, hypertension, tuberculosis, epilepsy or any other chronic illness.
No surgical history.
PERSONAL HISTORY:
Married, 2 daughters
Diet :mixed (consumes fish and meat)
Appetite: normal ( presently)
Sleep: disturbed
Bowel and bladder: normal
Addiction : betel, bidi, alcohol
Allergy: none
Hobbies: watching telivision
Daily routine:
The patient gets up early morning at 5am. After freshing up he takes water, one cup of lemon tea with biscuits. Then he rides his cycle almost around 5km to reach his bus stand where he is working as a bus driver. By 6:30 am he starts from Siliguri.
Sometimes he takes a 72 hrs shift (West bengal to Assam).
Around 9am he stops his bus for having breakfast which mainly includes rice,dal, vegetables or fish.
Next stop he takes around 1pm for lunch ( rice and fish).
His assistant takes up the driving duty from there. At 10pm they finally go for dinner in a restaurant which mainly includes rice ,dal,vegetables or fish.
Later he continues driving till next day morning.
FAMILY HISTORY:
Not significant
Clinical images:
Patient is conscious ,coherent and cooperative and well oriented to time, place , person.
Patient was examined in a well lit room after taking their consent.
Patient is undernourished.
Pallor- present
Icterus -absent
Cyanosis-absent
Clubbing-absent
Generalised Lymphadenopathy-absent
Edema-bilateral pedal edema present
VITALS
Temperature : 98.3℉
PR : 90 beats per minute
BP : 100/70 mm of Hg
RR : 22 cycles per minute
SpO2 : 96% room air
Systemic examination
Per abdomen:
Inspection-
Abdomen is distended , flanks are full, skin is stretched.
No visible peristalsis, scars, sinuses, hermial orifices.
Equal symmetrical movements in all quadrant’s with respiration.
Umbilicus: central
Palpation -
No local rise of temperature, no tenderness
All inspectory findings are confirmed by palpation, no rebound tenderness, gaurding and rigidity.
Liver and spleen not palpable.
No organomegaly
Fluid thrill present
Percussion:
Shifting dullness present
Auscultation:
CVS :
Jvp not raised
Inspection:
Shape of chest - elliptical
No visible pulsations
No engorged veins and scars
Apical impulse not visible
Palpation:
Apex beat present over the left 5th intercostal space 1cm medial to midclavicular line
No parasternal heave
No precordial thrill
No dilated veins
Auscultation:
S1 S2 heard ,No murmurs
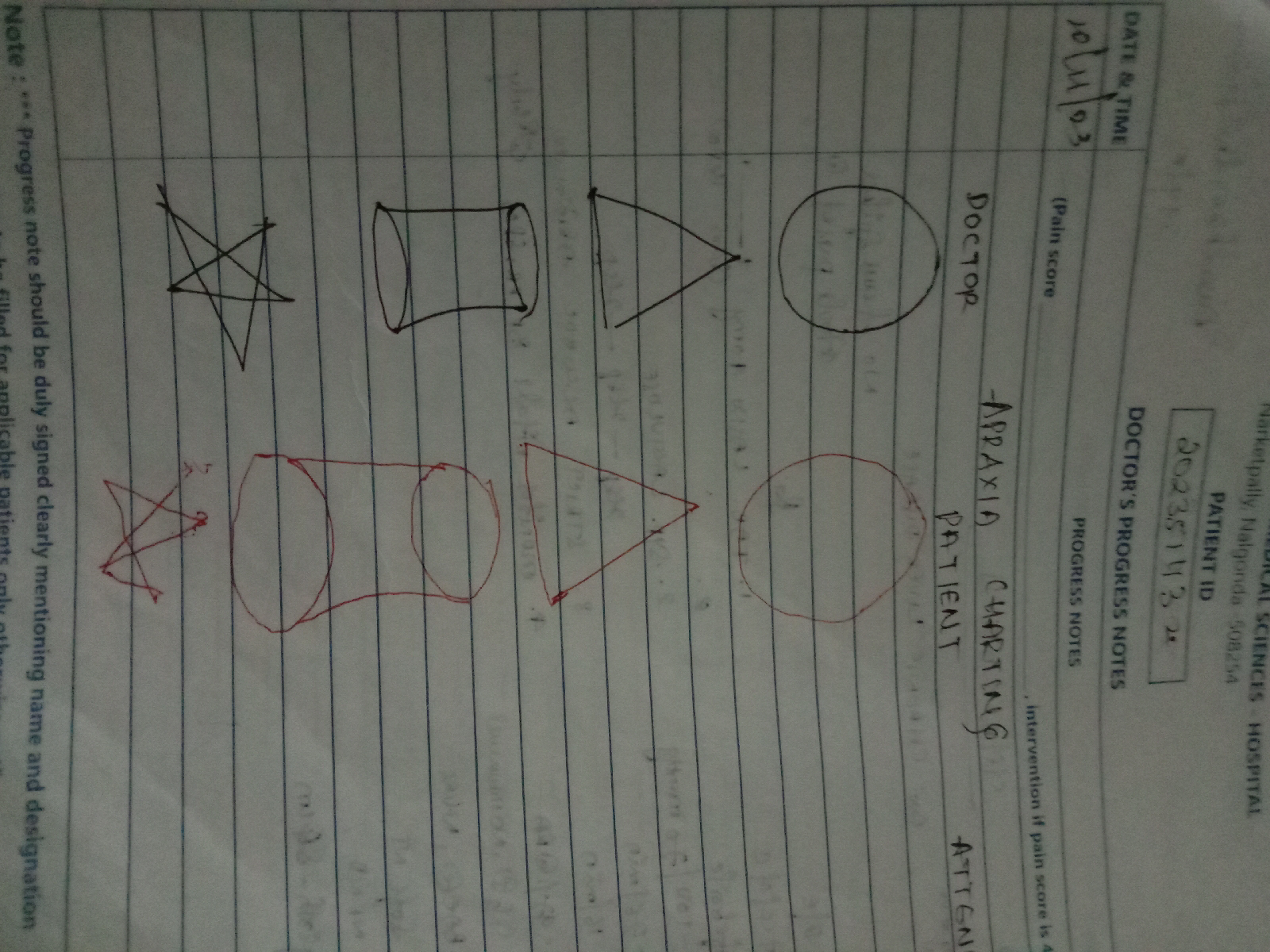
CNS:
No focal neurological deficits
Cranial nerves,motor and sensory functions intact.
RR:
Upper respiratory tarct - normal
Lower respiratory tract-
Inspection:
Chest bilaterally symmetrical,
Shape- elliptical
Trachea- Midline
Palpation:
Trachea is Midline
Normal chest movements
Vocal fremitus is normal in all areas
Normal vesicular breath sounds
No added sounds
shape of the chest: normal
Ascitic tap -
Appearance - clear , yellow coloured
SAAG - 1.65 g/dl
Serum albumin - 2.0 g/dl
Asctic albumin - 0.35 g/dl
Ascitic fluid sugar - 104mg/dl
Ascitic fluid protein - 0.7 g/dl
Ascitic fluid amylase - 17 IU /L
LDH : 143 IU/L
Cell count- 50 cells
Lymphocytes nil
Neutrophils 100%.
Provisional diagnosis:
Portal hypertension with ascites
TREATMENT :
Tab LASIX 40 mg PO BD
Syp. Lactulose 10 ml PO HS
Strict Alcohol abstinence .










Comments
Post a Comment