lekhana
51yrs old male with complaints of pain abdomen and vomitings
1) Pain abdomen since today morning
2) Vomiting
HOPI:-
Patient was appatently asymptomatic 3years back.He developed pain abdomen and vomitings for which he was diagnosed as acute pancreatitis at private hospital at nalgonda sanjeevani hospital, was admitted for 3days and subsided and got discharged. After 7 months he came to KIMS narketpally and got treated for some and got discharged at request and went to other hospital. Now patient came with abdominal discomfort and vomitings from today morning 8am
Past history:-
Is a known case of Dm is on Rx since 10-12years
Rx - T Glim m1 and T voglibose and glim m1
Is not a known case of HTN/CAD/Epilepsy
Is a known alcoholic occasional from 30years .stopped alcohol consumption since 3years
Personal history:-
Appetite -normal
Diet - Mixed
Bowels - regular
Micturition - Normal
No allergies
Family history:-
Not significant
General exmination
Patient is consious , coherent , well oriented to time , place and person
Patient is moderatley built and nourished
Pallor - no
Icterus - no
Cyanosis - no
Clubbing - no
Lympadenopathy- no
Malnutrition - no
Temp -98.6f
PR- 82Bpm
RR- 16cpm
Bp - 120/80
Spo2 - 98%
GRBS - 102 mg%
CVS -S1 S2 +ve
RS - Bae +ve
PS - Soft and non tender
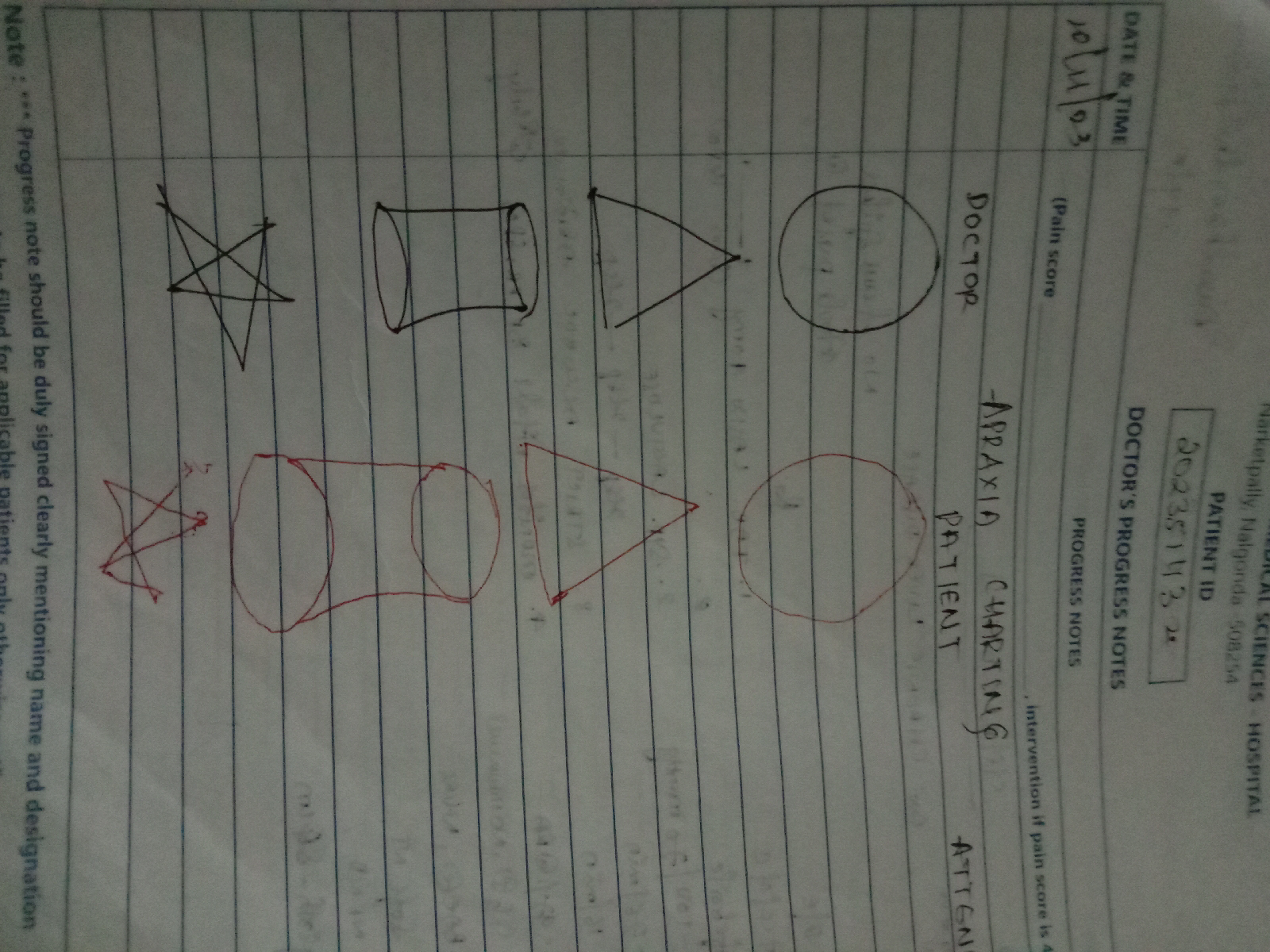
CNS - Higher motore functions intact
DIAGNOSIS:-
Pain abdomen under evaluation
Investigations